The Challenge of Diagnosing Catatonia in Autism and How Telemedicine Can Help
Once a family receives an autism diagnosis, often it is merely the beginning of a long string of conditions their child will have to battle throughout their life. A recent study found that over 95% of children on the autism spectrum have a co-occurring condition or symptom that can complicate their diagnosis and/or treatment. One condition that can be particularly challenging to diagnose is catatonia. Luckily for physicians and families, telemedicine may be able to meet the challenges of diagnosing this complex disorder.
What is Catatonia?
Dr. Amitta Shah, a consultant clinical psychologist with over 35 years experience working with patients with autism, describes catatonia as a “complex neuro-psychological disorder, which refers to a cluster of abnormalities in movement, volition, speech, and behavior.” Autism-related catatonia is generally marked by a change in behavior. Common signs include slowing down or freezing during actions, reduction in speech, and an odd or stiff gait. Though an estimated 12-18% of individuals with autism present with varying levels of catatonia, it is a difficult disorder to diagnose and treat. Though catatonia is treatable, if left untreated, catatonia is associated with significant morbidity and mortality.
Late Observance of Symptoms
One of the biggest challenges of diagnosing catatonia in autism is that the symptoms often overlap with those of an autism diagnosis. This means parents and clinicians should keep an eye out for a change in behavior. It is important to note that the onset of catatonic regression typically occurs at a later age than an autism diagnosis, most often during adolescence and young adulthood.
Misidentified, Misdiagnosed, and Mistreated
Because the symptoms of catatonia may be mistaken for those of autism, the disease is often left entirely unidentified, or misdiagnosed and then mistreated. Another reason for infrequent identification may be due to the fact that symptoms may not present while a child is visiting the doctor. And because these symptoms present gradually, clinicians may simply not be observing or recognizing them.
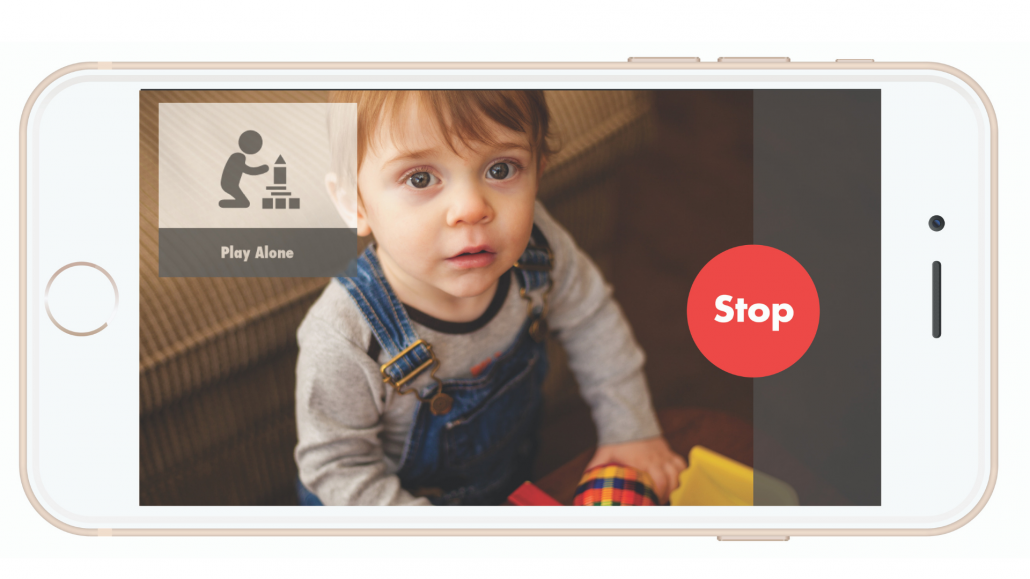
Can Telehealth Help?
For families seeking treatment, it can be frustrating to observe behaviors indicative of a condition that their doctor never witnesses. The solution may lie in telehealth. Remote monitoring technology such as Behavior Imaging can assist behavior specialists in documenting and detecting symptoms of catatonia. Videos of “behavior specimens” can be collected in the patient’s natural environment, and then securely shared between families and providers anywhere in the country. Once clinicians can see the symptoms of catatonia manifesting, they can more accurately and quickly diagnose the disease, allowing families to seek treatment options.
Creating a treatment plan after an autism diagnosis is a highly personalized and complicated process. In order to receive the best quality care, an accurate diagnosis of all co-occuring conditions, if any, is also vital. Click here to learn more about how telehealth can help with accurate diagnosis.