Provider Reimbursement Progress for Telehealth
It goes without saying that the CPT system of payments and coding is both complex and detailed. It involves payer codes, categories, circumstances of use, and time. This system came from a 1985 Harvard study that created the resource-based relative value scale. This scale deployed an ongoing method of calculating relative value units for physician services. Many practices utilize a third-party medical billing service to stay compliant and keep up with CMS changes that cycle every two years.
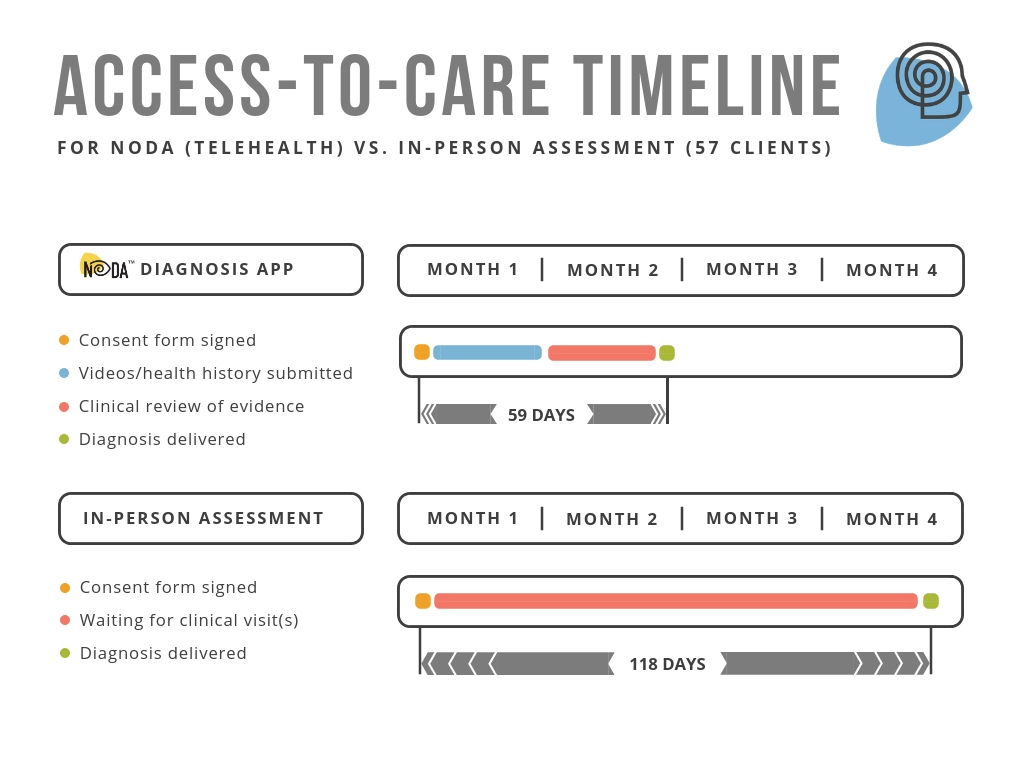
For 2019, CMS published ninety-nine CPT codes for telehealth services and specifically one new code that is exciting for us at Behavior Imaging in relation to our remote autism assessment tool, NODA (Naturalistic Observation Diagnostic Assessment). This article is an overview of those new codes and other emerging payment options that clinicians can use to expand telehealth services within their practice.
Direct Pay for Telehealth Services
One option for telehealth reimbursement is direct pay, wherein families pay the clinics directly for remote health assessment services. Families with health plan deductibles may be able to use the direct payment towards meeting their deductible.
For example, if the family’s plan deductible is $500 and the clinic charges $400 for a NODA assessment, the family direct payment for $400 would apply and meet 80% of their health insurance deductible. This method would allow a clinic to collect the direct payment in full and report the service and billable amount to the family insurer for tracking deductible spending. Of course, this method depends on the individual health plan of the family, but it can be a valuable tool for provider reimbursement.
Private Insurance Reimbursement
Private insurers follow CMS coding and payment schedules but can also incorporate their own payment schedules based upon needs and various state laws. The process varies by insurer and state. A few states and insurers have been open to emerging methods of evaluation and management. These progressive thinkers realize the benefits of technology that reduces both costs and wait-times. We suggest checking with the insurance providers in your state about the new and exciting changes outlined in the section below.
CMS Changes
In June 2017, the CPT Editorial Panel revised five existing codes, added 13 codes to provide better descriptions of psychological and neuropsychological testing, and deleted CPT codes 96101, 96102, 96103, 96111, 96118, 96119, and 96120. The RUC and HCPAC submitted recommendations for the 13 new codes and for the existing CPT codes 96105, 96110, 96116, 96125, and 96127.
The new coding structure separates billing for the first hour from each additional hour as well as distinguishes between evaluation services and test administration/scoring as follows:
- 96101 for psychological testing by a psychologist or physician is replaced by 96130 (first hour) and 96131 (each additional hour)
- 96136 for psychological testing evaluation and scoring services (first 30 minutes) and 96137 for test administration and scoring (additional 30 minutes)
Before the changes took effect on January 1, 2019, both CPT 96101 and CPT 96111 were used widely for Autism assessments.
ABA Assessment Code
The new ABA CPT code 97151 includes 15-minute billing increments for non-face-to-face analyzing of data as part of the behavior identification assessment. NODA can be incorporated into this assessment method as one of the tools used for evaluation reporting. The above changes are positive changes toward including NODA as one of the tools a clinical professional can utilize and be compensated within their practice.
New Exciting Reimbursement Code to Watch
For CY2019, CMS proposed to make separate payment for remote evaluation services when a physician uses pre-recorded video and/or images submitted by a patient in order to evaluate a patient’s condition through new HCPCS G-code G2010:
Remote evaluation of recorded video and/or images submitted by the patient (e.g., store and forward), including interpretation with verbal follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment
The new G2010 code was created with dermatology in mind, and although not specific to psychological testing, the fact that CMS considers this a viable and credible method of evaluation can only hold promise that NODA directly will correlate to expanding this service coverage for reimbursement in other categories. We hope to establish a working group to share both experience and patient results to CMS resulting in the expansion of this procedure for FY2021.
Increased Acceptance of Telehealth
New payer codes for telehealth services signal an increased acceptance of remote services and their benefits for both clinicians and patients. As clinics are able to treat more patients using cost-effective and evidence-based telehealth technology, we predict that it will become an essential part of every clinician’s toolkit.